Patients deserve to know what a given drug could cost when they’re being told about the benefits and risks it may have. They deserve to know if the drug company has pushed their prices to abusive levels. And they deserve to know this every time they see a drug advertised to them on TV. — Alex Azar, The National Academy of Medicine, 10/15/18
Remember when pharmaceutical executive Martin Shkreli became the symbol for pharmaceutical greed by hiking the price of an infection treatment from $13.50 to $750 overnight? Or outcry when the price of EpiPen skyrocketed from $90 to more than $600?
While both are extreme examples, large jumps in prescription drugs prices are nothing new. A recent Kaiser poll found one in four people taking prescription drugs have difficulty affording their medication and the issue receives bipartisan support for government action.
Priority 3: Lowering Prescription Drug Costs
So it came as no surprise when the Department of Health & Human Services made lowering the costs of prescription drugs a top priority along with value-based care transformation, combating the opioid crisis, and healthcare access and affordability.
Key Priority Areas
As part of their focus, HHS is looking at several problems that plague drug markets, including:
- High list prices
- Seniors and government programs overpaying due to lack of negotiating tools
- Rising out-of-pocket costs for consumers
- Foreign governments benefitting from American investment in innovation
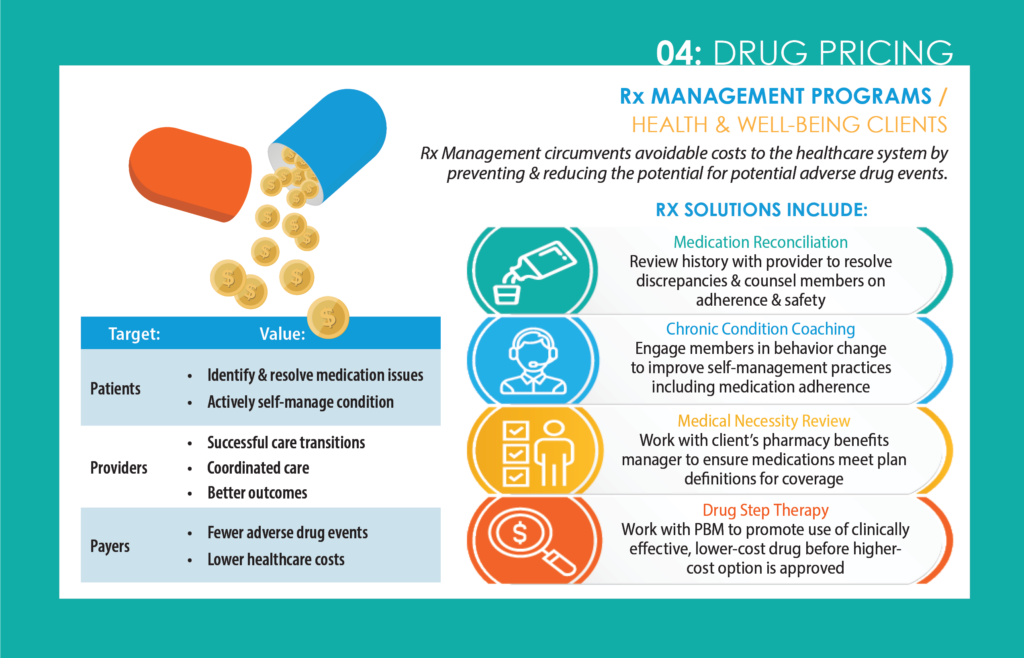
Although Telligen cannot directly impact market prices, we do help our clients implement strategies for helping our clients lower spending, improve engagement, raise satisfaction, increase care coordination, and reduce the potential for adverse drug events. Examples include:
Medication Reconciliation
Review history with provider to resolve discrepancies and counsel members on adherence and safety.
Chronic Condition Coaching
Engage members in behavior change to improve self-management practices including medication adherence.
Medical Necessity Review
Work with client’s pharmacy benefits manager to ensure medications meet plan definitions for coverage.
Drug Step Therapy
Work with pharmacy benefit managers to promote the use of clinically effective, lower-cost medication before the higher-cost option is approved.